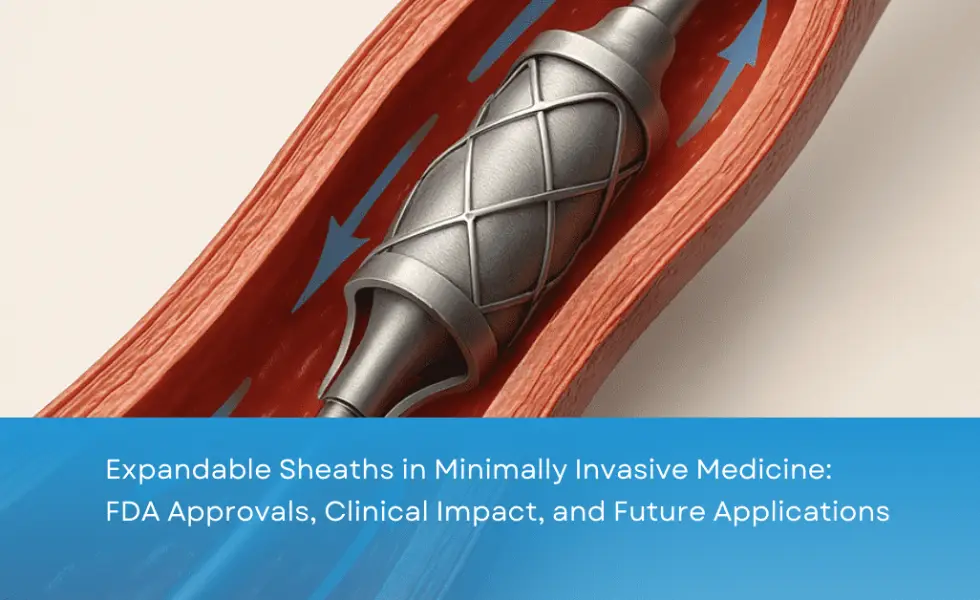
Expandable sheaths are reshaping minimally invasive medicine. By allowing larger devices to be delivered through smaller access sites, they make procedures safer and recovery faster. Once limited to a handful of uses, these devices are now expanding into new clinical fields—improving outcomes for patients, surgeons, and healthcare systems alike.
What Are Expandable Sheaths in Minimally Invasive Medicine?
Expandable sheaths are introducers that can widen inside the vessel after insertion. This flexibility allows larger devices to be inserted without causing trauma to the artery. Their main advantage is reducing vascular complications such as bleeding, dissection, and stenosis, while maintaining procedural efficiency.
FDA-Approved Expandable Sheaths for Minimally Invasive Procedures
Several devices are already FDA-approved and in wide clinical use:
Medtronic Solopath™ Balloon-Expandable Sheath – FDA-cleared in 2018 for TAVR. Trial data showed a 52% reduction in vascular complications compared to standard sheaths.
Edwards Lifesciences eSheath® – FDA-approved for Sapien 3/Ultra valves. The PARTNER 3 trial showed a 40% reduction in major vascular complications.
Gore DrySeal Flex Introducer Sheath – FDA-approved for TEVAR/EVAR. Registry studies reported a 35% lower rate of access-site hematomas.
Clinical Impact of Expandable Sheaths
Expandable sheaths improve outcomes across multiple procedures:
TAVR – Vascular complications reduced from 10–15% to 5–7%, with shorter ICU stays.
TEVAR/EVAR – Access-site injury reduced from 8–12% to 4–6%.
Lead extraction – Vascular trauma cut in half, lowering procedural mortality.
Fewer complications mean fewer transfusions, faster recovery, and shorter hospitalizations.
Future Applications of Expandable Sheaths
The potential of expandable sheaths extends beyond current uses:
TMVR (Transcatheter Mitral Valve Replacement): Could cut iliac artery injuries by half.
Peripheral artery interventions: Projected to lower complication rates from up to 18% to around 8%.
Pediatric procedures: Smaller expandable sheaths may reduce femoral artery stenosis to 2–4%.
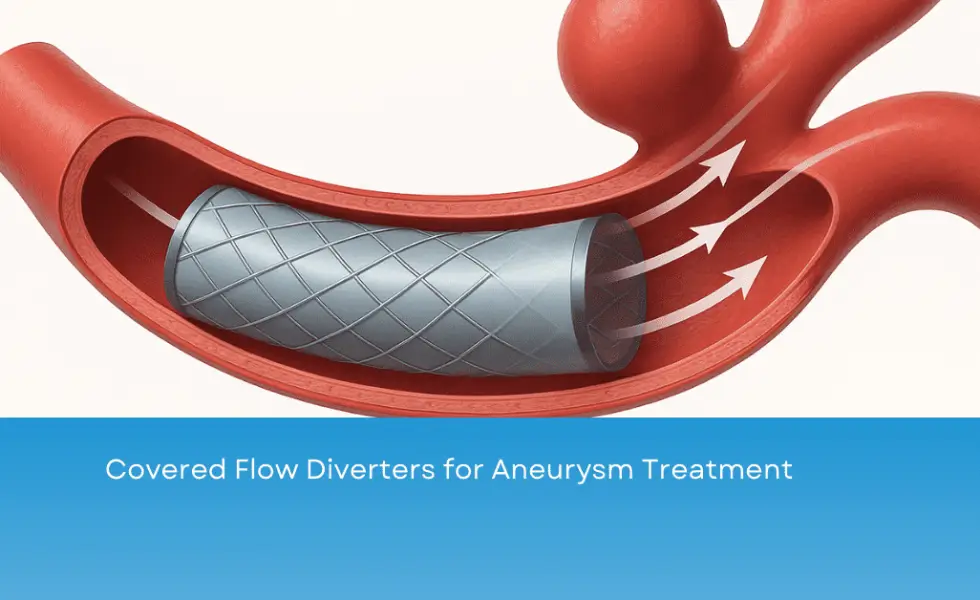
Neurovascular interventions: Controlled expansion could lower embolism risk to 2–3%.
High-risk PCI: Safer delivery of mechanical support devices with fewer vascular injuries.
Benefits for Patients, Surgeons, and Healthcare Systems
Patients – Faster recovery, fewer complications, shorter hospital stays.
Surgeons – Easier procedures, less risk of vascular injury, reduced operating time.
Healthcare systems and insurers – Lower readmission rates and cost savings of $3,000–5,000 per case.
Challenges and Barriers to Adoption
Despite clear benefits, adoption of expandable sheaths faces:
Higher upfront cost (20–30% more than standard sheaths)
Need for surgeon training in expansion techniques
Limited compatibility with all devices
Ongoing innovation and cost reduction are expected to broaden adoption.
Conclusion
Expandable sheaths in minimally invasive medicine are a game-changer. FDA-approved devices already show dramatic reductions in vascular complications, and expanding their use could prevent thousands of complications annually. Patients recover faster, surgeons gain procedural confidence, and healthcare systems save costs—highlighting the transformative potential of this technology.